By the term arthroplasty we refer to the creation of a new artificial joints. It is a very common orthopaedic surgical operation and concerns mainly bigger joints such as the hip and the knee. Less frequently, arthroplasty can be performed on the shoulder, the ankle and knuckle.
Arthroplasty can be partial or total, in other words it either concerns one part of the joint or both parts. Materials used can be made of metal, plastic or in some cases ceramic.
With normal activity these materials should have a lifetime of 15-20 years providing the procedure has been successful.
It is the ultimate solution for patients aged 60-80 years, offering them an improved quality of life free of pain.
This operation is absolutely necessary when a joint is in the final stage of damage due to various reasons (osteoarthritis, rheumatoid arthritis, post traumatic arthritis etc.).
It is the last resort when all conservative methods have failed.
The first hip replacement took place in 1960 and is still considered one of the most successful surgical operations in Medicine. Since 1960 frequent improvements in technology as well as surgery have increased the effectiveness of the operation. Today, more than 1,000,000 surgical operations of this kind are performed around the world.
ANATOMY
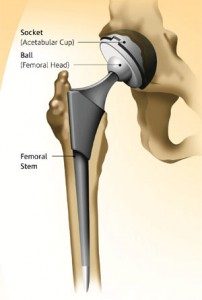
The hip joint is one of the larger joints of the body. It is formed by the acetabulum, which is part of the pelvis, and the femoral head. The femoral head, which looks like a ball, is inserted into the socket (acetabulum) to form the joint.
The surface of the joint is covered by cartilage (soft and smooth tissue with a low friction factor). Between them there is synovial fluid that helps the friction generated with movement.
The joint is covered by the joint sac, which is a thin, but hard coating which produces the lubricant synovial fluid and gives stability to the joint.
PATHOGENY
Arthritis (osteoarthritis, rheumatoid arthritis and post traumatic arthritis) is the most common cause of deterioration of a joint.
Osteoarthritis
It is a form of arthritis relating to deterioration due to ageing. This usually occurs in individuals over 50 or in individuals with hereditary conditions. The cartilage gradually deteriorates until the bones start to rub against each other, causing pains in the hip and hindering movement. Osteoarthritis can even be caused due to irregularity of the formation of the hip during childhood (congenital dysplasia of the hip).
Rheumatoid Arthritis
It is an autoimmune condition where the joint membrane displays an intense inflammation and thickening. This chronic inflammation gradually destroys the joint cartilage causing acute pain and stiffness.
Post Traumatic Arthritis
This appears after trauma of the joint surface as a result of a fracture (intra joint fracture of the acetabulum or the femoral head)
Aseptic Necrosis
A trauma of the joint, such as a dislocation or fracture, can cause damage to the blood supply of the femoral head. The resulting absence of blood supply will lead to the collapse of the cartilage followed by arthritis. In addition, circulation related disorders as well as other conditions can result in aseptic necrosis.
Hip Joint Conditions in Childhood
Some newborn babies display dysplasia of the hip joint. Even though it can be dealt with using modern methods, they will go on to present arthritis later in life.
Total arthroplasty of the hip is an orthopaedic surgical procedure that should only be performed when arthritis is in its final stage. The age of the patient is a very important parameter in the decision of whether the operation can be performed due to the fact that the materials used have an estimated lifespan of 15-20 years.
It is an operation that puts an end to chronic unbearable joint pains and at the same time almost completely restores the function of the joint.
Candidate patients for such an operation should meet the following criteria:
- Be under 80 years of age.
- Be in fairly good physical condition and self-sufficient.
- Be mobile and energetic.
- Not have serious health problems.
- Be suffering for over 6 months from frequent and chronic pain in the area of the hip, which doesn’t diminish with analgesic medicine and affects daily activities.
Technical Data
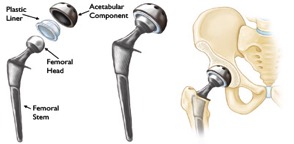
The artificial join comprises of 4 parts
- Femoral stem
- Femoral head
- Acetabular component
- Plastic liner
The implants are made of various alloys which are high pressure resistant and durable (titanium, chromium, cobalt, steel, ceramic and plastic)
Pre Operation Plan
- Patient’s history
- Lab tests
- Cardiological tests
- Pelvis, hip and chest x rays – technical measurements
- Provision for 2-3 units of blood for transfusion.
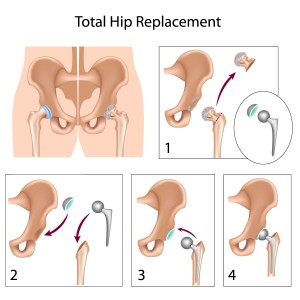
Method of Surgery
The operation is performed under general or epidural anaesthesia. The surgeon gains access to the joint through a small incision (10 cm). The deteriorated acetabular joint surface is revealed and cleaned with a special tool (reamer) until the bone is uncovered. Then, the acetabular component is inserted with its plastic liner. Afterwards, an osteotomy is performed on the femur and the femoral head is removed. Following that, the bone lumen is prepared, in other words, a gap is created in the femur where the femoral implant will be placed. Finally, the artificial femoral head is placed at the end of the created gap followed by the reset of the joint (femoral head into the acetabular component). Now a new artificial joint has been created. The functionality of the joint is tested before the wound is stitched.
The following day drainage tubes are removed and the patient is mobilized with the help of a physiotherapist, who helps the patient take a few steps.
The patient remains in hospital for a maximum of 4 to 5 days and then returns home with guidelines.
Post–Surgery Progress
The patient must strictly follow these instructions given by their orthopaedic surgeon:
- Take anticoagulant medication
- Take analgesics
- Elevate your toilet and bed
- Use a medical walker
- Have physiotherapy
- Avoid extreme movements of the hip (deep squats, leg crossing etc.)
COMPLICATIONS
The percentage of complications after a hip replacement is low and includes:
Infection
The infection can be superficial or internal. It can occur at any point of time, from hospitalization up to a few years later.
Minor infections can be dealt with using antibiotics. Infections that have reached or affected the implants can result in their removal, and replacement at a later time. Any infection in the body can cause the arthroplasty to be rejected.
Vein Thrombosis of the Lower Limbs
This is the most common complication after a hip replacement. Blood clots can form on the leg and be transported to the lungs, causing a pulmonary embolism. The danger is minimized with the use of anticoagulant medication and mobilization of the patient.
Leg length discrepancy (LLD)
A possible complication after an arthroplasty operation is that the limb can be shorter or longer than the healthy one. During a surgical procedure, measurements are made and every precaution is taken to ensure that both limbs will retain their length. In the unlikely case of failure, a correction is made by using shoe lifts for the shorter limb.
Hip Joint Dislocation
This happens when the femoral head comes out of its socket (acetabulum). This can be caused by an extreme movement of the hip, as well as after an unsuccessful operation due to inappropriate surgical methods being followed. It is more likely to happen during the first few months after the operation, while surrounding tissue is still in healing process. It can be relocated with a special technique and in the case that there is a relapse, the patient needs to undergo a further operation surgery that is known as revision surgery.
Slackening and Deterioration of Materials
This usually happens after a number of years and is down to wear and tear of the material due to extensive use. If the slackening is painful, a revision surgery on the joint replacement will be necessary
Joint replacement of the hip is an orthopaedic surgical procedure that puts an end to chronic pain from arthritis. With the right pre operation plan, the correct method, implants of excellent quality and adherence to the surgeon’s advice, it can be a very successful operation that will improve the quality of life of the patient.